Diabetes, also called; diabetes mellitus is a disease in which the body’s ability to produce or respond to the hormone insulin is impaired, resulting in abnormal metabolism of carbohydrates and elevated levels of glucose in the blood and urine. Consult a doctor for medical advice
Most common types
- Type 2 diabetes: A chronic condition that affects the way the body processes blood sugar (glucose).
- Type 1 diabetes: A chronic condition in which the pancreas produces little or no insulin.
- Prediabetes: A condition in which blood sugar is high, but not high enough to be type 2 diabetes.
- Gestational diabetes: A form of high blood sugar affecting pregnant women.
Type 2 diabetes
Type 2 diabetes, also called: adult onset diabetes is a chronic condition that affects the way the body processes blood sugar (glucose). Very common, more than 3 million US cases per year. With type 2 diabetes, the body either doesn’t produce enough insulin, or it resists insulin. Symptoms include increased thirst, frequent urination, hunger, fatigue, and blurred vision. In some cases, there may be no symptoms. Treatments include diet, exercise, medication, and insulin therapy.
Type 1 diabetes
Type 1 diabetes, also called: juvenile diabetes is a chronic condition in which the pancreas produces little or no insulin. Common with more than 200,000 US cases per year. It typically appears in adolescence. Symptoms include increased thirst, frequent urination, hunger, fatigue, and blurred vision. Treatment aims at maintaining normal blood sugar levels through regular monitoring, insulin therapy, diet, and exercise.
Prediabetes
Prediabetes, also called: impaired glucose tolerance is a condition in which blood sugar is high, but not high enough to be type 2 diabetes. Very common with more than 3 million US cases per year. Without intervention, it’s likely to become type 2 diabetes within 10 years. Many people with prediabetes have no symptoms. Progression from prediabetes to type 2 diabetes isn’t inevitable. With lifestyle changes, weight loss, and medications, it’s possible to bring a blood sugar level back to normal.
Gestational diabetes
Gestational diabetes, also called: diabetes during pregnancy is a form of high blood sugar affecting pregnant women. Common with more than 200,000 US cases per year. Those who develop gestational diabetes are at higher risk of developing type 2 diabetes later in life. In most cases, there are no symptoms. A blood sugar test during pregnancy is used for diagnosis. Treatment strategies include daily blood sugar monitoring, a healthy diet, exercise, and monitoring the baby. If blood sugar is too high, medication is needed.
Economic and Well-Being Impact
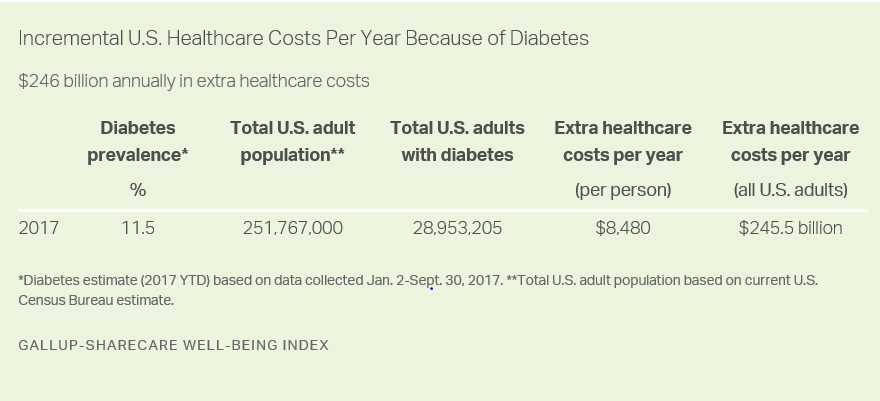
According to the Gallup-Sharecare Well-Being Index™, the national prevalence of diabetes increased from 10.6% in 2008 to 11.5% for the first nine months of 2017. This increase has had a direct impact on health care costs and health outcomes.
If the diabetes rate had remained at its 2008 level, approximately 2.3 million fewer U.S. adults would have the disease today, and healthcare costs due to diabetes would be an estimated $19.2 billion less than current levels. Costs to employers are significant with more than $20 billion annually in lost productivity, stemming from 57 million additional unplanned missed workdays by workers with diabetes.
Further, the residents of the U.S. communities with the highest prevalence of diabetes have higher rates of obesity, high blood pressure, high cholesterol, heart attack and depression and are less likely to engage in healthy behaviors than residents in the lowest prevalence communities.
This Gallup and Sharecare research also examines diabetes and its relationship to key well-being and productivity outcomes. It also addresses how health systems are leveraging best practices to expand diabetes management both within the hospital setting and out to the communities they serve.
Diabetes Costs U.S. Economy Estimated $266B Annually
- Diabetes adds estimated $245.5 billion annually in healthcare utilization
- Increase in diabetes rate since 2008 has added $19.2 billion to 2017 costs
- Higher absenteeism costs employers an extra $20.4 billion annually
Diabetes among American adults is estimated to cost the U.S. economy an additional $245.5 billion in 2017 in total healthcare expenditures. These results are based on the diabetes rate of 11.5% thus far in 2017 and are coupled with an estimated incremental healthcare cost of $8,480 per person compared with those who have not been diagnosed with diabetes.
These data are drawn from more than 135,000 interviews with U.S. adults across all 50 states and the District of Columbia so far in 2017 as part of the Gallup-Sharecare Well-Being Index. These findings are from a report released today, The Cost of Diabetes in the U.S.: Economic and Well-Being Impact.
The estimates for the incremental healthcare utilization costs per person, which have been adjusted for inflation, are drawn from research by the American Diabetes Association. The extra costs per person per year have been conservatively computed by the ADA to account for overlapping costs of other chronic conditions commonly associated with diabetes.
Since 2008, the national adult diabetes rate has risen nearly one percentage point, elevating the current cost estimates. If the diabetes rate had remained steady at 10.6% since that time, the estimated healthcare expenditures due to diabetes in 2017 would be about $19.2 billion less than they currently are.
Diabetes Linked to Increased Workplace Absenteeism
Diabetes costs the U.S. economy in more ways than just extra healthcare utilization. One such way is lost productivity in the form of unplanned absenteeism, which costs U.S. employers an estimated $20.4 billion annually.
The diabetes rate thus far in 2017 is 6.3% among full-time workers and 9.1% among part-time workers. Full-time workers with diabetes miss an average of 5.5 extra workdays per year, and part-time workers with diabetes (after reducing to half-day estimates) miss an additional 4.3 days. This amounts to nearly 58 million additional days of unplanned missed work each year among workers who have been diagnosed with diabetes, compared with their counterparts who do not have diabetes.
Assuming a cost of $354 per day for the average worker across occupations, lost productivity due to absenteeism related to diabetes costs employers $20.4 billion annually. This analysis controls for age, gender, income, education, race/ethnicity, marital status, children in household, geography and BMI weight class.

Implications
Diabetes has become a major health problem in the U.S., resulting in significant costs to the U.S. economy. And healthcare utilization and unplanned absenteeism are only two potential ways that chronic conditions such as diabetes can affect it. Other ways not examined in this article include actual performance while at work, voluntary and involuntary turnover, and workers’ compensation claims.
The slow climb in diabetes prevalence of about one percentage point over the past decade mirrors the three-point climb in obesity, which has been found to quadruple the risk of diabetes for working-age U.S. adults. Among workers, the occurrence of diabetes is not evenly distributed across occupations, nor are its risks. Transportation workers have both the highest current rate of diabetes and the highest risk for new onset diabetes in the future, posing unique challenges for this industry.
According to the Centers for Disease Control and Prevention, 86% of the nation’s $2.7 trillion in healthcare expenditures comes from people with chronic and mental health conditions, underscoring the critical nature of both managing disease states when they are present and preventing them in the first place.
Population health programs such as Blue Zones Project in California’s Beach Cities have a proven track record of reducing above-normal weight and smoking rates while boosting exercise and healthy eating. These behaviors play a role in reducing reports of diabetes diagnoses among residents.
Employers, too, can play a decisive role in their workers’ lives by establishing incentives, recognition systems and workplace cultures designed to promote active living and healthy choices.
And hospitals and health systems serve a vital purpose in diabetes and glycemic management, which can improve health outcomes and lower the costs of care — both inpatient and outpatient — for people with diabetes. Opportunities exist for hospitals and health systems to partner with local employers to bring diabetes education and prevention to work sites.
“While most clinicians agree that managing diabetes improves health and reduces medical costs, the benefit to employers also extends to a more productive workforce,” says Sheila Holcomb, vice president, Sharecare Diabetes Solution. “An opportunity exists for employers to partner with the medical community, specifically Certified Diabetes Educators at local and regional hospitals, to offer diabetes education and training to their employees with diabetes. This collaboration has tangible and proven value for both the individual and the company’s bottom line.”
Download the full report
Gallup-Sharecare The Cost of Diabetes in the U.S.: Economic and Well-Being Impact
Gallup-Sharecare The Face of Diabetes in the United States
The overall diabetes rate and estimated healthcare costs are based on 135,426 telephone interviews with U.S. adults across all 50 states and the District of Columbia, conducted Jan. 2-Sept. 30, 2017. The missed-work estimates among workers are based on 80,136 interviews with full- or part-time workers conducted Jan. 2-Oct. 15, 2017. Gallup conducts 500 telephone interviews daily, resulting in a sample that projects to an estimated 95% of all U.S. adults.
The margin of sampling error for diabetes prevalence for all U.S. adults is ±0.2 percentage points, while the margin of error for full-time workers is ±0.3 points and the rate for part-time workers is ±0.6 points. All reported margins of sampling error include computed design effects due to weighting.
Each daily sample of national adults in 2017 includes a minimum quota of 70% cellphone respondents and 30% landline respondents. Additional minimum quotas by time zone and within region are included in the sampling approach.
The partnership between Gallup and Sharecare merges decades of clinical research, health care leadership and behavioral economics expertise to track and understand the key factors that drive greater well-being for individuals and populations.
Well-being is a concept that captures the important aspects of how people feel about and experience their daily lives — encompassing more than just physical health or economic indicators, well-being includes five elements: purpose, social, financial, community, and physical.
The Gallup-Sharecare Well-Being Index is the world’s largest data set on well-being, with over 2.5 million surveys fielded to date. The Well-Being Index provides unmatched, in-depth insight into the well-being of populations, is frequently cited by national media, and has been leveraged by Nobel laureates and academicians for peer-review and scholarly articles. Gallup interviews 500 people every day; the result is a sample that projects to an estimated 95% of U.S. adults.
Previously known as the Gallup-Healthways Well-Being Index, the Gallup-Sharecare Well-Being Index™ was recently rebranded following Sharecare’s 2016 acquisition of Healthways. This rebrand signifies a new and exciting union of the powerful insights generated by Gallup and the meaningful health engagement fostered by Sharecare, to create a healthier world through knowledge, information and action.